Advanced neurosurgical techniques
Neurosurgical techniques, particularly those involving vascular interventions require both technical expertise and advanced fluorescence imaging technology. To enhance surgeons' skills, pre-surgery imaging techniques such as 3D-CT, along with technologies that support visualization during surgery, including motor-evoked potential (MEP) and fluorescent imaging (ICG), are crucial for achieving safe and satisfactory outcomes in neurosurgical procedures. Simultaneous and clear visualization of blood flow in neurovascular procedures is one of the most important challenges of neurosurgery.
Case 1: Anterior choroidal artery bifurcation aneurysm - Protecting blood flow in the anterior choroidal artery (AChA) through fast clipping
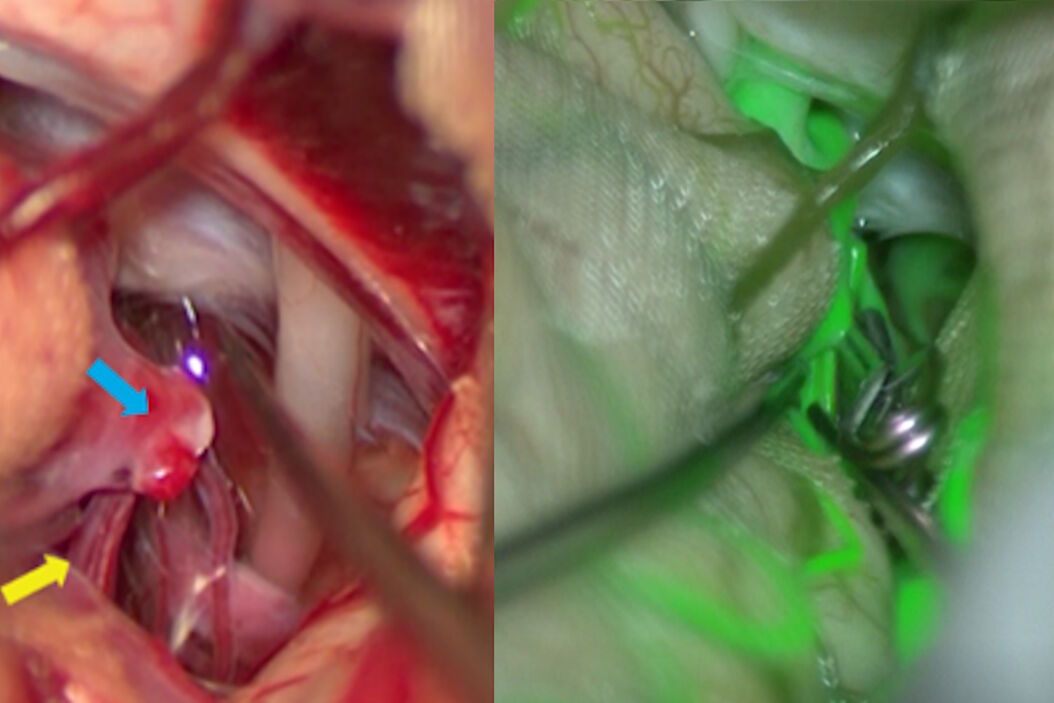
In this case the anterior choroidal artery, a small perforating artery, poses a significant challenge during brain aneurysm surgery. This artery, with a diameter of just 1 mm, is often obscured or positioned behind an aneurysm and difficult to identify and to protect during the clipping procedure. As obstruction of the AChA can lead to serious complications such as hemiplegia or homonymous hemianopsia, it is critical to preserve these arteries (Fig. 1A).
For the clipping of the anterior choroidal artery bifurcation aneurysm, Prof. Mizutani used a technique where the clip blade is manipulated delicately with 3-dimensional movements, maintaining sight of the tip until the end of clipping (Blading technique [1,2]). To monitor the blood flow in the perforating branch, the GLOW800 3D AR fluorescence application delivered an augmented view of real-time vascular flow directly in the natural white light visualization. As with the classic black and white ICG, GLOW800 AR allows blood flow to be visualized in real-time even for vessels of around 1 mm. Blood flow, the location of the aneurysm clip and the perforator (AChA) can be checked at the same time as each other, without any sensation of shift or latency. The significant volume of information obtained from this single image facilitates decision-making.
After the initial clipping, decreased blood flow in one of the two AChA can be observed using GLOW800 (Fig. 1B). Immediate clip re-positioning was consequently performed by Prof. Mizutani to restore the blood flow (Fig. 1C-D).
Case 2: Large vertebral artery aneurysms - treatment of partially thrombosed large vertebral artery aneurysm with large amounts of information
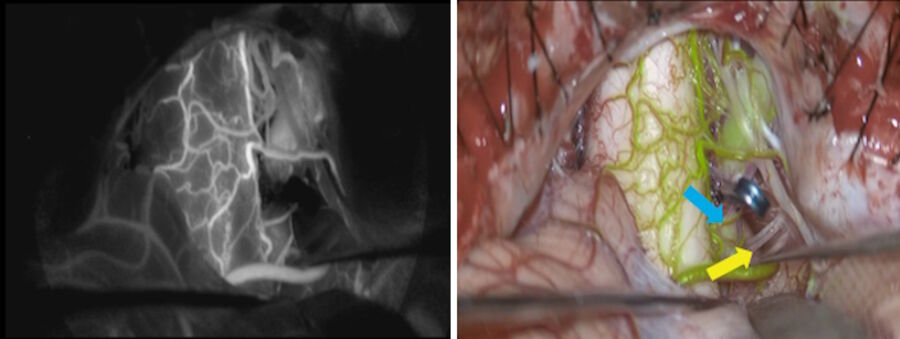
A partially thrombosed large vertebral artery aneurysm is a condition where a vertebral artery progressively enlarges, forming an aneurysm. As the aneurysm grows, it compresses the lower cranial nerves and the medulla oblongata, often causing dizziness and difficulty swallowing (dysphagia). The surgical treatment is challenging. It is key to protect the brain stem and lower cranial nerves, as well as preserving the perforating arteries.
Surgical proximal parent artery occlusion (PAO) is one of the treatments for partially thrombosed vertebral artery aneurysms (PTVAs). It avoids nerve damage and fully evaluates the perforating branches to the brain stem [3] intraoperatively.
While brain stem, nerves, and blood vessels can be identified through conventional intraoperative indocyanine green video angiography, the perforator blood flow cannot be seen (Fig. 2, left). The GLOW800 AR application delivers enhanced information and helps the proper assessment of the perforator blood flow to the brain stem and the clipping can be completed while maintaining direct sight of the brain stem, nerves and blood vessels. (Fig. 2, right).
Conclusion
In neurovascular interventions, precise 3D visualization of cerebral anatomy and real-time blood flow is paramount to achieving optimal surgical outcomes. Prof. Mizutani’s vascular cases demonstrated the benefits of the GLOW800 Augmented Reality fluorescence 3D application from Leica Microsystems. This technology integrates real-time visualization of blood flow with anatomical structures, providing an augmented 3D view with depth perception. Such innovation enhances intraoperative decision-making, particularly during critical phases of aneurysm clipping, allowing surgeons to precisely position clips with confidence.
Disclaimer
The statements of the healthcare professionals included in this presentation reflect only their opinion and personal experience.
Not all products or services are approved or offered in every market and approved labelling and instructions may vary between countries. Please contact your local Leica representative for details.
Images are courtesy of Professor Tohru Mizutani, Chief Professor of the Department of Neurosurgery at Showa University, Japan.