1. Initial Patient Presentation and First Surgery
Patient:
A 58-year-old female, with a medical history of well controlled hypertension presented with confusion and complete left hemiparesis.
Diagnosis:
- A ruptured right MCA M1 aneurysm
- Unruptured left MCA and PCOM aneurysms
- Her only medications were antihypertensives.
Treatment decision:
The decision was made to urgently treat the ruptured right MCA aneurysm with microsurgical clipping, in order to protect the patient from rebleeding from the unstable aneurysm.
The unruptured aneurysms were on the contralateral side and needed another craniotomy. Therefore we opted to wait for full recovery from the first surgery and subsequently treat the unruptured aneurysms with microsurgical clipping.
Outcome first surgery: Treatment of the ruptured right MCA with microsurgical clipping
The surgery on the ruptured right MCA aneurysm was successful and she was discharged 24 days post op. At the time of her discharge she had recovered the strength in her left leg and arm, but the left facial weakness remained. The cardiologist that evaluated her during hospitalization maintained her previous medications, with good control of her hypertension.

2. Pre-Operative Assessment Before Second Surgery
Three 3 months after the first surgery to treat the right-sided ruptured MCA, the patient returned for microsurgical clipping of the unruptured left MCA and PCOM aneurysms. Her physical examination at this time showed her to have a good general appearance, no cardiac abnormalities or signs of peripheral vascular compromise, or other signs of disease. Her neurological examination showed persisting left central facial weakness but no other neurological abnormalities, including of the cranial nerves.


The following images show the injection of the left ICA. We can see both aneurysms in the 3D reconstruction. Since we had both a PCOM and an MCA aneurysm to treat, we decided on a Transsylvian approach, through a Pterional craniotomy.




3. Intra-Operative Course and Images
We performed a Pterional craniotomy with the withdrawal of the lesser sphenoid wing. With this craniotomy, we exposed the superior and part of the middle temporal gyrus, the Sylvian fissure, and the inferior and part of the middle frontal gyrus. For the approach, we opened Sylvian fissure, separating the frontal lobe from the temporal lobe, where we could find the MCA with its branches (and the aneurysm on the M1 segment). On the proximal M1 MCA, we entered the carotid cistern, where we could find the MCA and the PCOM aneurysms. Prof. Feres Chaddad opened the Sylvian fissure using sharp dissection, maintaining the dissection on the arachnoid space.
Pre-Clipping
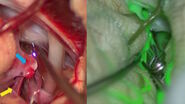
Identification of MCA & PCOM aneurysms with GLOW800 Augmented Reality Fluorescence from Leica Microsystems
Before clipping, GLOW800 helped to see the flow running through all the vessels and the aneurysms. GLOW800 also helped to distinguish the areas that were thrombosed, on the MCA aneurysm.
After the recognition of the main structures – ICA, ACA (A1), optic nerve, PCOM, choroidal arteries, and MCA (M1 and M2 branches) – the PCOM aneurysm was clipped. It is vital to be sure that both PCOM and the anterior choroidal arteries are preserved.
We then performed the occlusion of the MCA aneurysm. When this aneurysm was clipped we had to be sure that the superior and inferior trunks of M1 did not have a kink or a torsion that could lower the flow in these vessels.
Post-Clipping Videos
Visual confirmation of clip position with GLOW800 Augmented Reality Fluorescence from Leica Microsystems
Post clipping, GLOW800 was fundamental to show the patency of the PCOM and the anterior choroidal arteries, as well as the superior and interior trunks of MCA. GLOW800 is an instant tool to check the flow distal to the clip, which allows one to continue to work during its acquisition, even positioning the clip.
4. Post Surgery



Post Surgery Examination and Discharge
- GCS 15, pupils equal, round, and reactive to light
- Left central facial weakness
- Normal motor function with muscle strength 5/5 bilaterally
- She was discharged 4 days post surgery
5. Impact of GLOW800 Augmented Reality Fluorescence in Aneurysm Treatment
One augmented view during vascular neurosurgery improves confidence in intra-operative diagnosis
- One augmented, real-time view means no more need to recall and try to reconcile the black and white blood flow video with the natural anatomical view
- Crisp delineation helps you limit potential compromise or obstruction of surrounding perforators and small vessels
- Full depth perception and no dark peripheries supports clear spatial orientation to aid manipulation of vessels

Improved confidence in treatment
Visualization with GLOW800 AR supports each step of vascular neurosurgery procedures and also supports with post-operative imaging. For example during aneurysm clipping, it helps:
- Confidently apply an aneurysm clip
- Assess clip placement and aneurysm occlusion
- Check if all branches proximal and distal to the clipped aneurysm are perfused and whether there is orthograde filling of the blood vessels
- Confirm the clip has not caused any compromise of surrounding blood vessels, such as kinking or partial obstruction

A fundamental tool for the future practice and training in neurosurgery
In the binocular image injection (CaptiView) better defining (lowering) the dose of Indocyanine Green (ICG) was enough to generate the flow effect without saturating the view of the whole operative field. Also the microscope’s monitor offers a perfect view, where the observer can easily understand the anatomy and the clipping strategy adopted. Image settings can be effortlessly changed, to optimize the view as needed.

Download
Download Case Study GLOW800 Augmented Reality Fluorescence in Aneurysm Treatment (pdf, 2,4MB)