Background
The current consensus to achieve safe and favorable treatment outcomes in glioma surgery is “maximal safe resection” which involves removing as much of the tumor as possible without causing neurologic deficit.
Even if the boundaries of the tumor can be identified based on preoperative MRI, for the tumor width or span, the practical problem is the identification of the bottom area, which is left to the surgeon's judgment.
5-ALA, which is used in intraoperative fluorescence diagnostics, has been approved because it contributes to maximal safe resection and overall survival (OS). However, it should be noted that more data needs to be accumulated, and further discussion is required in the future regarding its features, capabilities, and method of use.
Conventional intraoperative fluorescence diagnostics has the disadvantages of low excitation light, unclear boundaries, and surgery must be performed while constantly switching to white light, because of lack of anatomical information in dark conditions due to the use of blue light. It is the cause of eye fatigue in the surgeon. The GLOW400 AR fluorescence was developed in response to the demand of having all information available in one single screen.
Case study
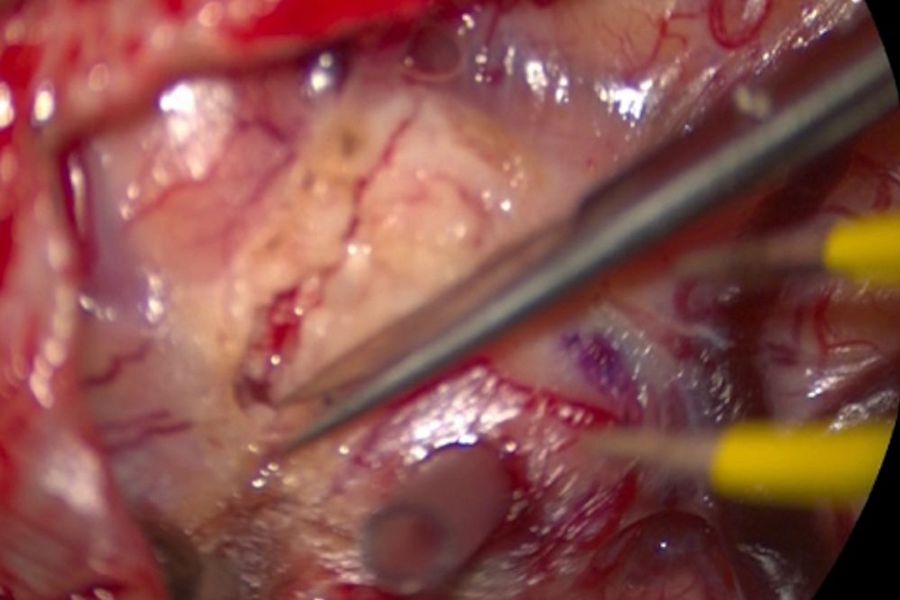
As the tumor was being resected, strong fluorescence was achieved, and the surrounding vessels could also be identified. For delicate procedures, we switched to normal white light as needed, but the switching could be done within 1.5 to 2 seconds.
Video 1: GLOW400 Anatomy mode, starting from white light mode. Video courtesy of Prof. Kondo.
Video 1: GLOW400 Anatomy view. Video courtesy of Prof. Kondo
Simultaneously check surrounding structures and boundaries
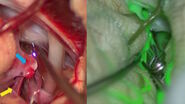
Considering the properties of 5-ALA, techniques that avoid excessive tumor resection are needed, and the fence-post technique is a useful method to achieve that (Fig. 3).
Video 2: GLOW400 Anatomy mode, starting from white light mode. Video courtesy of Prof. Kondo.
In this case, as the area around the fence-post was opened up, fluorescence was observed near the fence-post, which were clearly visible.
And we were able to perform a surgery where the boundaries were clearly identifiable. The “Anatomy View” allows for finding boundaries while also checking surrounding structures (Fig. 4).
About Evolved ARveo 8
At Leica Microsystems, we aim to navigate the evolving landscape of neurosurgery with you using our advanced AR technology. Our ARveo 8 ecosystem, integrates the ARveo 8 digital visualization microscope, GLOW800 and GLOW400 3D clinical applications, and the MyVeo surgical visualization headset.
Download
Disclaimer
This document is a rewrite of the co-hosted Afternoon Seminar at the 82nd Annual Meeting of the Japanese Society of Neurosurgery. The statements of the healthcare professionals included in this presentation reflect only their opinion and personal experience. Not all products or services are approved or offered in every market and approved labeling and instructions may vary between countries. Please contact your local Leica representative for details.