Introduction
PVR surgery is especially challenging for a host of reasons, including the reduced countertraction for membrane removal against detached retina, the risk for creating additional retinal holes, hemorrhage, or inflammation that can generate new PVR, and the high likelihood of requiring prone positioning postoperatively to keep the retina attached. PVR may appear as prominent, white, fibrotic tissue with infolding of adjacent retina creating a classic “star fold” appearance. It may also manifest as thin sheets without obvious distortion. Incomplete removal of PVR may prevent retinal attachment or lead to recurrent RD after silicone oil tamponade is removed. Therefore, PVR should be removed as completely as possible to maximize the chances for permanent retinal attachment.
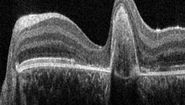
Visualization of PVR poses the greatest limitation to its complete removal. PVR may be translucent or opaque and stains poorly with triamcinolone, indocyanine green, or trypan blue, particularly when there are anterior membranes. Intraoperative optical coherence tomography (OCT) imaging facilitates complete detection of PVR membranes through real-time, high-resolution mapping.6 OCT can identify surgical planes to initiate peeling, confirm adequacy of peeling, and indicate when a deep forceps grab is engaging the retina. From a practical perspective, mapping can be performed either by serial volume scans in areas of suspicion based upon retinal folds or retinal vessel obscuration, or by driving raster scans around the fundus for continuous feedback for either targeted or comprehensive mapping. It is highly recommended to repeat such scanning after membrane removal to confirm its adequacy and completeness before infusing gas or oil tamponade.
Case Description
A 4-year-old girl was accidentally shot with a blunt-tipped metal arrow into her orbit resulting in a traumatic retinal detachment of the right eye (OD) that was initially successfully repaired with scleral buckling. Five months later, she returned with declining vision in her right eye from a macula-involving tractional retinal detachment (TRD) associated with contraction of the posterior hyaloid face and grade C1 proliferative vitreoretinopathy (PVR) (Figure 1). A 25-gauge pars plana vitrectomy with membrane peeling was performed to repair the TRD OD (see the Surgical Video section below).
Intraoperative OCT was particularly useful in evaluating the multiple surgical planes of the split posterior hyaloid face (PHF), including a layer of retained PHF over the posterior and peripheral retina that partially stained with triamcinolone acetonide (Surgical Video). After release of traction along a radially oriented retinal fold that was partially supported by a high posterior scleral buckle, the presence of a star fold involving the fovea was confirmed by OCT (Surgical Video). As the membrane was peeled, the stress on the fovea was monitored by OCT to prevent macular hole formation. The membranes were successfully removed, and the macula gradually reattached over the next few weeks (Figure 2).
Conclusions
Proliferative vitreoretinopathy (PVR) remains a major obstacle for long term success in retinal detachment surgery. The primary treatment of PVR is surgical, and near-complete membrane removal is necessary to reattach the retina. Intraoperative OCT is a critical new tool for intraoperative surgical decision making in PVR surgery through identification of membrane location, tractional effects on the retina, and surgical planes for membrane peeling. The Proveo 8 ophthalmic microscope with EnFocus HD OCT from Leica Microsystems provides high resolution images that define how PVR alters the vitreoretinal interface. Real-time OCT scanning can monitor for stress on the retina during membrane peeling and confirm the adequacy of membrane removal to reach a surgical endpoint. In summary, intraoperative OCT can improve surgical outcomes by more complete membrane removal with less iatrogenic retinal trauma.
Video
About Dr. Robert Sisk

Robert Sisk, MD is Associate Professor of Ophthalmology at the University of Cincinnati. He is a Vitreoretinal Surgeon and partner at Cincinnati Eye Institute and serves as Director of Pediatric Retinal Surgery and Director of Ophthalmic Genetics at Cincinnati Children’s Hospital. He completed a Vitreoretinal fellowship at Bascom Palmer Eye Institute after his Ophthalmology residency at University of Cincinnati. He is a principal investigator for numerous clinical trials with interests in gene and cell therapy, macular degeneration, and diabetic retinopathy.