Neurosurgery in Sub-Saharan Africa: Challenges & Progress
Whereas neurosurgery has developed quickly in high income countries, the situation is different in middle and low-income countries. In many cases, neurosurgery was not considered a priority and there was a misconception that results were poor. However, the situation is now changing even though there is still a deficit of neurosurgical care in middle and low-income countries, and especially in Sub-Saharan Africa.
One of the issues is the deficit of neurosurgeons. Efforts have been made to improve neurosurgery training in Sub-Saharan Africa. This includes the creation of the World Federation of Neurosurgical Societies (WFNS) Rabat Training Center (RTC), established in 2002. This increased the number of neurosurgeons in Sub-Saharan Africa from 79 in 1998 to 369 in 2016.
Dr. Karekezi’s Journey to Establish a Neurosurgical Department within the Rwanda Military Hospital
Like many other African countries, Rwanda has a shortage of neurosurgeons. In 2011, when Dr. Karekezi started her neurosurgery training in Rabat, there were only 2 neurosurgeons in Rwanda for 11 million people. There are now 6 neurosurgeons in the country for 12 million people. An additional 114 neurosurgeons are needed to reach the 1:100.000 ratio recommended by the WHO.
During her training, Dr. Karekezi acquired knowledge and skills, she recounts, and learnt planning and adaptability. She then went on to do a fellowship in Toronto, which provided good learnings on having dedicated Operating Rooms with adequate instruments such as navigation and a surgical microscope.
Coming back to her country, Dr. Karekezi initiated the Neurosurgery Department within the Rwanda Military Hospital. The beginnings were challenging, with only 2 neurosurgeons and no residents. There was a critical care team with shared ICU beds, no dedicated Operating Room and shared ward beds. The team only had simple instruments to treat complex cases, such as trauma and large brain tumors.
The role of supporting teams is essential. This includes emergency physicians, anesthesia and critical care specialists and ICU nurses as well as supporting specialties: radiology, neurology, pathology, oncology and ophthalmology. Communication, respect and teamwork have been critical success factors to make the collaboration work.
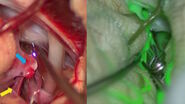
According to Dr. Karekezi, continuous mentorships and connections are important to gain insight on complex cases, progress and learn about advanced techniques, such as awake surgery. Building solid collaborations with expert neurosurgeons for training is also key, such as the one established between the Rwanda Military Hospital and Prof. Sébastien Froelich from France.
Establishing a Neurosurgical Department: Needs & Key Success Factors
A good approach, dr. Karekezi explains, is to think in terms of 4Ss: system, staff, space and stuff (equipment). Then, it is critical to look at how to build-up human resources and increase diagnostic tools (CT scanners, MRIs, microscopes, etc.). Limited resources also require practical and cost-effective solutions (endoscopy, pocket ultrasounds, shunts, etc.). In addition, there is a need to raise awareness about the specialty and position neurosurgery as a key member of global health.
Modern neurosurgical equipment can be very expensive. Overcoming this challenge means looking for affordable options, prioritizing, upgrading progressively and maintaining what exists. Good visualization is paramount. It gives neurosurgeons tools to perform better surgeries, allows them to take on more difficult cases and enhances patient safety. In addition, it also provides a platform for training. Technology is one of the pillars of the provision of healthcare.
Want to learn more? Register below to watch the full webinar presented by Dr. Claire Karekezi.
Note: The statements of the healthcare professional in this video reflect only her opinion and personal experience. Her statements do not necessarily reflect the opinion of any institution with whom she is affiliated.