Webinar Content
Spinal Arterio-Venous Fistulas: Preliminary Considerations
It is essential for the neurosurgeon to have a good understanding of the arterial vascular anatomy of the spine and of the circulation of the dural sleeve. The artery of Adamkiewicz, which supplies two thirds of the lower spinal cord, plays an important clinical role. An occlusion of this artery during surgery can cause a spinal infarction, also called anterior spinal artery syndrome, resulting in a loss of function of the anterior two thirds of the spinal cord and motor paralysis below the level of the lesion. It is also vital for the neurosurgeon to have a good knowledge of the venous vascular anatomy of the spine. The veins of the spine and of the cord have many anastomoses, which create a network of more than one anterior and posterior spinal vein.
Spinal Arterio-Venous Fistulas: The Spetzler Classification System & Epidemiology
The Spetzler classification of arterio-venous malformations of the spine distinguishes four different types:
- Type 1, representing 80% of cases, includes all dural arterio-venous fistulas (AVF)
- Type 2 are glomus arterio-venous malformations (AVM)
- Type 3 refers to juvenile arterio-venous malformations
- Type 4 are pial arterio-venous fistulas
Type 1 is divided into 3 sub-groups:
- Extradural arterio-venous fistulas, for which the treatment is usually non-surgical
- Dorsal intradural arterio-venous fistulas, which represent 80% of dural arterio-venous fistulas and for which the treatment could either be surgical or endovascular
- Ventral intradural arterio-venous fistulas, addressed with endovascular treatment
In addition, it is important to distinguish low flow and high flow dural arterio-venous fistulas, which have different pathomechanisms and clinical symptoms. Most patients present with slowly progressing symptoms of myelopathy.
Dorsal Intradural Arterio-Venous Fistulas [1,2,3]
Dorsal intradural arterio-venous fistulas are a rare condition. The incidence is 5 to 10 cases per 1 million inhabitants per year. Around 80% of patients are male and the mean age is 55 to 60 years. The most prevalent localization is at the thoracic level, which is slightly more common than the lumbar level. Fistulas at the cervical level are very rare, and only occur in around 2% of cases. Given the low incidence rate, there are currently no prospective randomized multicenter studies.
Spinal Arterio-Venous Fistulas: Treatment and Surgical Approach [4,5,6,7]
Before treatment, a preoperative evaluation is performed including an evaluation of the neuro-status and urodynamic status, a spinal MRI and spinal digital subtraction angiography.
An individual treatment plan is established for each patient. Endovascular treatment is often feasible, with very low morbidity under 1%. However, according to various studies, the obliteration rate is only around 50% and as such, many patients then require surgery. As a first step, it often makes sense to offer interventional treatment and, if it is unsuccessful, move to surgical treatment. Surgical treatment of dural arterio-venous fistulas is more invasive but very effective, with an obliteration rate of 98%. The morbidity is slightly higher than with endovascular treatment, at around 2%.
Treatment strategies often tend to be center-specific. For example, the Kiel hospital does one embolization trial and if it is not successful, an early surgical obliteration is performed. Time is critical: delayed treatment can lead to the aggravation of symptoms with less responsiveness to treatment.
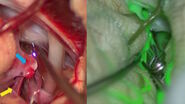
After patient positioning in the operating room, a partial laminectomy is performed. It allows to see the nerve route exiting the spinal canal. The neurosurgeon then opens the dura to operate on the fistula. ICG intraoperative angiography is performed before and after occlusion of the fistula. It can help localize the intradural draining vein and verify fistula obliteration.
Surgical treatment leads to a stabilization or improvement of symptoms in 92% of patients. Motor symptoms improve for two thirds of patients while sensory deficits improve in one third. There is a strong association between pre and postoperative status. Patients with mild symptoms tend to recover very well, while recovery is longer for patients with more severe symptoms.
Note: The statements of the healthcare professional in this video reflect only her opinion and personal experience. Her statements do not necessarily reflect the opinion of any institution with whom she is affiliated.
References
- Koch MJ, Stapleton CJ, et al., Open and endovascular treatment of spinal dural arteriovenous fistulas: a 10-year experience, (2017) JNS. 26(4): 519-523
- Tsuruta W, Matsumaru Y, et al., Clinical Characteristics and Endovascular Treatment for Spinal Dural Arteriovenous Fistula in Japan: Japanese Registry of Neuroendovascular Therapy 2 and 3, (2019); NeurolMedChir. (Tokyo). 59(12): 492-497
- Krings T, Geibprasert S., Spinal dural arteriovenous fistulas, (2009); AJNR. 30(4): 639-648
- Van Dijk JM, TerBrugge KG, et al., Correlation between time to diagnosis and rehabilitation outcomes in patients with spinal dural arteriovenous fistula, (2002); Stroke. 33(6): 1578-83
- Niimi Y, Berenstein A, et al., Spinal Dural Arteriovenous Fistulas, (1997). Neurosurgery. 40: 675-82.
- Eskander EN, Borges LF, et al., Spinal dural arteriovenous fistulas: Experience with endovascular and surgical therapy, (2002);JNS. 96(2): 162-7.
- Steinmetz MP, Chow MM, et al., Outcome after the treatment of spinal dural arteriovenous fistulae: a contemporary single-institution series and meta-analysis, (2004). Neurosurgery. 55(1): 77-87.