Key learnings
- Learn about the concepts and rationale of Epidural Lateral Approaches in skull base neurosurgery
- Discover surgical techniques and fields of application
- Watch videos of clinical cases
Speaker
Prof. Pierre-Hugues Roche
Prof. Pierre-Hugues Roche is a Professor of Neurosurgery at the Medical School of Marseille in France. He is also the Chief of the Department of Neurosurgery at the University Hospital of Marseille North and President of the skull base section of the French Neurosurgery Society. Prof. Roche is involved in research activities on skull base surgery and spine trauma.
Epidural Lateral Approaches: concepts & rationale
The cisternal approach has a number of advantages for skull base tumors and diseases: it is a familiar anatomy; it provides a natural corridor and is easy to enter and to leave. However, it has some disadvantages such as exposure of the brain, vessels and nerves as well as delayed bleeding control. This can make it difficult to achieve a complete radical resection.
The use of the petrosal approach allows surgeons to mimic skull top surgery for skull base tumors. It shortens the working distance and allows the lesion to be devascularized first. It can also limit retraction of the tissues and manipulation of the brain and the nerves. This can enable a better radical resection if needed. Collaboration with the ENT surgeon is often useful for these procedures. However, there are some disadvantages too; this approach has a steep learning curve and surgery can be longer. The bone work can also be difficult to evaluate, and each bone work carries its own risk.
The paradigm is changing, with a shift towards “functional sparing” skull base neurosurgery. This is fueled by a better assessment of complications, increased understanding of tumor biology, the emergence of quality-of- life evaluations and the introduction of alternative treatments.
Epidural Lateral Approaches: surgical techniques & fields of application
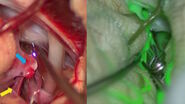
Epidural Lateral Approaches rely on several surgical techniques: anterior petrosectomy, epidural resection of the anterior clinoid process (ACP) and combined petrosectomy (posterolateral approach).
Identifying the best approach for each lesion in skull base tumors and vascular diseases depends on several factors: the goal of the surgery; the location, size and extent of the tumor; the patient’s condition including his age and general health condition as well as the team’s experience.
These techniques can be used for both skull base diseases and regular diseases, such as aneurysms. In some cases, it is possible to associate approaches, such as the transpetrosal and transylvian approach also called the half-and-half which can for example be useful for meningiomas. Another valuable combination is the anterior petrosectomy and transcavernous approach.
There can be complications, as with any approach. They can be hard to predict due to parameters that are difficult to foresee such as vascularization, texture and adhesion. To limit complications, patient selection and the neurosurgeon experience play an essential role. In addition, complex approaches are not always necessary and conventional approaches and radiosurgery can be quite effective in some cases.
Want to learn more? Register to watch the full webinar presented by Prof. Pierre-Hugues Roche and see the different clinical cases he shared.
Note: The statements of the healthcare professional in this video reflect only his opinion and personal experience. His statements do not necessarily reflect the opinion of any institution with whom he is affiliated.